Welcome Members
Get connected to your health with the MySanfordHealthPlan member portal.
New member? Get started
Sanford Health Member Portal
Your MySanfordHealthPlan member portal- NOW in MyChart, makes managing your health care easier than ever!
Log InDon’t have an account?
Request an ID Card
Access Wellness Tools
Check Benefit Balances
View Claims
Find a Provider or Pharmacy
Pay My Premium
Member resources
Understanding Your EOB
Knowing how to read an Explanation of Benefits (EOB) is helpful to understanding your health insurance.
Learn MoreMy rights
You have rights, and we are committed to resolving your concerns if an issue arises.
Prior authorization
Learn more about the prior authorization process and what services require prior authorization.
Learn MorePharmacy information
Learn more about pharmacy benefits and details on medication policies, coverage, participating pharmacies, and more.
Learn MoreMembers FAQs
How can I access my 1095-B tax form?
The Affordable Care Act, or ACA, required you to provide proof of health insurance coverage when filing your taxes. Recent changes to the law mean that you are no longer required to provide proof of coverage forms when filing your taxes. However, should you want one of these forms, they are still available to you through Sanford Health Plan.
Get a Form 1095-B from Sanford Health Plan. You can receive a copy of the 1095-B upon request. There are three ways to get this form:
1. Send an email to memberservices@sanfordhealth.org to request your 1095-B
2. Call our Customer Service team at (800) 752-5863 to request your 1095-B
3. Mail a request for your 1095-B to:
Attn: Customer Service
Sanford Health Plan
P.O. Box 91110
Sioux Falls, SD 57109-1110
You have the right to receive a form 1095-B within 30 days of your request.
What pharmacies can I use to fill my prescriptions?
Pharmacies that have contracted with OptumRx, on behalf of Sanford Health Plan are considered to be participating pharmacies. You can find a listing of participating pharmacies. If you choose to go to a non-participating pharmacy, you will have to pay full-price for the prescription, rather than your copay.
How do I know what expenses my HSA or FSA covers?
When you participate in a Health Savings Account (HSA) and/or Flexible Spending Account (FSA), you’re able to contribute pre-tax funds for use on hundreds of eligible expenses. Recently, you gained even more flexibility in your ability to save when the CARES Act was signed into law.
This new legislation expanded the list of expenses that are considered eligible by including popular over-the-counter products, which consumers can now purchase with their HSA or FSA without a prescription. This change went into effect on January 1, 2020, and allows over 20,000 new expenses as eligible moving forward. That’s great news for consumers, since the average American shops for over-the-counter medications 26 times each year. For more information, click here.
What if I need to see a specialist?
Sanford Health Plan does not require a referral from your primary care physician to see a specialist who is in the network. If the specialist is NOT a participating provider, you must contact Sanford Health Plan to request authorization. If authorization is received, your benefits will be considered In-Network. Failure to obtain prior authorization may result in reduced coverage to the specialty services.
What if there aren't participating providers in my residential area?
Sanford Health Plan has contracted with other networks for those members who reside, travel or attend school outside the Sanford Health Plan service area. If you have an additional network listed on your identification card, you may seek medical care from a provider that is participating with the additional network. If these additional networks do not provide you with access to a needed provider, the Sanford Health Plan Access and Availability rules will apply. Please refer to your Policy for details. You can find the links to the additional networks available to you here or by calling Member Services at 1-800-752-5863. If you have questions or do not have access to our website and would like to request a printed provider Directory, please call Member Services. IMPORTANT: If you choose to go to a non-participating provider when in network access is available, your claims will be paid according to your out-of-network benefits.
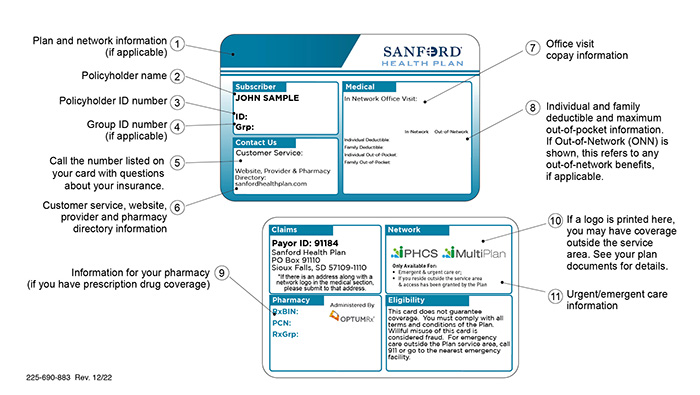
What does all of the information on the front and back of my ID card mean?
The policyholder of the coverage will receive one (1) ID card if they have single coverage and two (2) ID cards if others are also on the plan. Haven't received your ID card? Lost your ID card? Log in to your Member Portal to view or print a temporary card or request a new one. If you need to fill a prescription and do not have your ID Card, pay for the medication and submit a paper claim to the plan for reimbursement.