Explanation of Benefits
After a members claim is processed, Sanford Health Plan sends the member an EOB outlining the charges that were covered. We also notify the health care professionals of the covered charges.
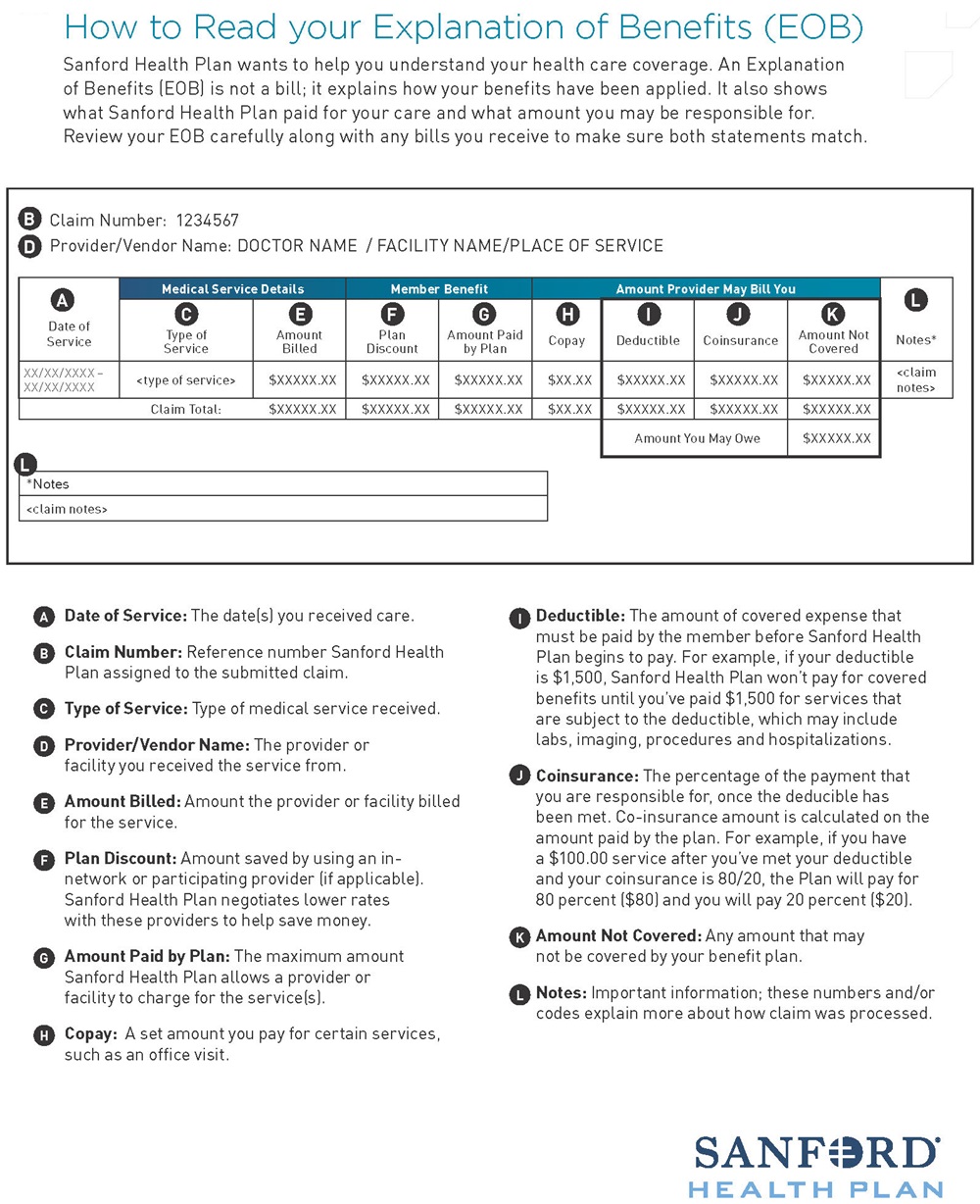
The following picture describes important terms used in the member Explanation of Benefits (EOB) and throughout the claims payment process. Reviewing this will help the member become familiar with these terms in order to better understand their benefit plan.
The purpose of an EOB is to show the benefits coverage the member received for the services billed to Sanford Health Plan by the members health care Practitioner and/or Provider. The Explanation of Benefits shows the dollar amount of services that were billed by the member’s Practitioner and/or Provider and how that amount is applied to deductible, coinsurance or copayments, or if any of the charges were for non-covered services. Members will be able to clearly see the amount they owe to the provider. Members can sign up (through their secure online member account) for electronic EOBs to reduce the amount of paper mail.